Fighting Fat with Fat
When we think of ways to lose weight, our first approach is usually to reduce dietary fat. However, certain fats may actually aid weight loss through their lipid-lowering and anti-inflammatory effects.

When we think of ways to lose weight, our first approach is usually to reduce dietary fat. However, certain fats, including the naturally occurring omega-7, monounsaturated fatty acid (MUFA), cis-palmitoleic acid (POA), may actually help through their lipid-lowering and anti-inflammatory effects.1
The amount of POA is relatively low in plant and marine based foods, but abundant in macadamia nut and sea buckthorn oils,1 where it accounts for roughly 17 percent2 and up to 35 percent3 of fatty acids, respectively. Although most adults typically eat only about 2 g/d of POA,4 it is the second most abundant MUFA in most blood lipids and is a key substrate for triglycerides synthesis,5 hence it is concentrated in fat tissue. Within the body, it is predominantly made from surplus dietary carbohydrate,6 or through desaturation of palmitic acid via steroyl-coenzyme A desaturases (SCDs),7 including SCD1 primarily found in fat and liver. SCD1 and its products are important contributing factors in obesity, and therefore, its activity is often measured and reported as a desaturation index where the ratios of POA to palmitic acid and of oleic acid to stearic acid are quoted.5 This intricate role of POA between carbohydrate and fat metabolism suggests its importance in weight management.
Health benefits of POA were first discovered through human studies more than a decade ago, where simply adding macadamia nuts to the diet6 consistently and significantly decreased total and low-density lipoprotein (LDL) cholesterol regardless of initial cholesterol status.8,9,10 Currently, results of in vitro studies provide the most consistent measure of POA action, showing it suppresses fat synthesis and enhances energy expenditure, which increases fat breakdown and reduces fat storage.1,7,11 Within pancreas tissue, it increases insulin secretion and insulin content,12 and the total number of insulin producing β-cells,13 thereby improving fat cell response to insulin, which improves glucose metabolism and regulates fat storage.12 For blood sugar control, it works about half as well as a drug approved for diabetes treatment.14
Animal study results add weight (pardon the pun) to the in vitro evidence. Obese animals given POA acid generally have reduced circulating insulin levels, increased insulin sensitivity, smaller fat cells with less fat content resulting in less adipose tissue deposition and resistance to diet-induced weight gain. In genetically diabetic/obese mice, dietary POA supplementation increases pancreas weight and decreases plasma glucose and insulin levels, improves insulin-signaling which increases glucose transport into skeletal muscles and improves glycemic control and insulin resistance, partly by suppressing lipogenic and inflammatory gene expression.13 It also reduces food intake and body weight.13 Similar results occur in obese sheep where intravenous infused PAO reduces circulated insulin levels and improves insulin resistance through altering gene expression specifically in muscle tissue, for genes regulating glucose uptake and fat burning.7 Such treatment reduced intramuscular fat cell size, total fat content within fat cells and weight gain by 77 percent in a dose dependent manner as the blood concentration of POA increases.7 In addition, increased levels of the hormone cholecystokinin, which promotes a feeling of fullness, combined with decreased food intake was observed in male rats given dietary POA.15
How POA may produce similar benefits in humans is only now being elucidated and proving to be exceedingly complex. That’s partly because most POA within the body is de novo synthesized from carbohydrate rather than originating from direct intake, and additionally because POA has been measured in various lipid fractions from different tissues or blood lipids, and the mechanisms responsible for its presence in those fractions is poorly understood. Some epidemiological studies report that higher blood POA is associated with higher markers for metabolic syndrome,16 body mass index (BMI),6 abdominal fat deposits and obesity,5 and less successful weight maintenance after weight loss.6 However, because POA accumulation in certain tissues may result from excess carbohydrate intake, this may be a consequence rather than a contributing factor to obesity. If so, the anti-obesity effects of dietary POA observed in animal models still warrants further investigation in humans.
To date, human intervention trials assessing the impact of dietary POA on obesity and metabolic syndrome risk are lacking. Those including macadamia nut8,9,10 and sea buckthorn oils17,18,19,20,21 provide enticing yet weak evidence of potential benefits including anti-inflammatory and lipid lowering effects. Unfortunately, both oils contain bioactive compounds in addition to POA including tocopherols, carotenoids and phytosterols.2,3 As a consequence, it is difficult to know whether observed health benefits are solely due to POA. In addition, both contain significant quantities of palmitic acid, shown in preclinical studies to counter the beneficial effects of POA. Therefore, trials including purified POA products would enable more robust conclusions.
Currently, only one commercially available purified POA test material has been assessed in human intervention trials.6 Use of the product as a food ingredient has received no objection from FDA based on a generally recognized as safe (GRAS) notification (GRAS Notice 494). It is an ethyl ester concentrate derived from sustainable Peruvian anchovy, manufactured using a patented process to contain not less than 50 percent POA and not more than 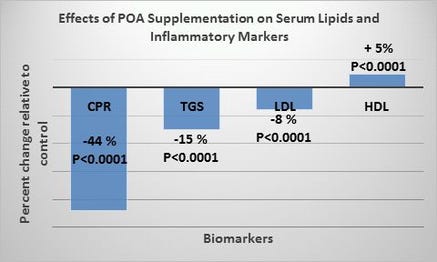 1 percent palmitic acid. It provides more POA as a percentage of total fatty acids compared to macadamia or sea buckthorn oils, lacks non-fatty acid bioactives and has little potentially interfering palmitic acid.
1 percent palmitic acid. It provides more POA as a percentage of total fatty acids compared to macadamia or sea buckthorn oils, lacks non-fatty acid bioactives and has little potentially interfering palmitic acid.
A randomized, double blind, placebo-controlled trial including this purified POA, reported highly significant lipid lowering and anti-inflammatory effects in 60 adults with dyslipidemia and high C-reactive protein (CRP), which is a marker for inflammation.6 Compared to placebo, 220.5 mg/d POA reduced CRP by 44 percent, blood triglycerides by 15 percent and LDL cholesterol by 8 percent, and increased high density lipoprotein (HDL) cholesterol by 5 percent (Figure 1).
These consistent and highly significant results contributing to cardiovascular health and potentially benefiting fatty liver disease and obesity risk, emphasize the need for further larger and longer term studies assessing the impact of purified POA on specific end points including weight loss. These more robust investigations will establish POAs role, efficacy and safety in the fight against metabolic syndrome including cardiovascular disease and insulin resistance that is associated with diabetes and obesity.
Nancy Morse's 33-year career in lipid research included quality control (QC), clinical and R&D laboratory management, and establishment of a blood fatty acid database instrumental in identifying abnormalities in lipid metabolism specific to unique disease states. She was a director of the NS Life Sciences Industry Association and the Canadian Health Foods Association, has co-authored over 35 peer-reviewed articles, and has spoken at universities and public venues in nearly two dozen countries including as a guest on radio and television talk shows.
Looking for more information on how to fight fat with fat?
Nancy Morse will speak on “Fighting Fat with Fat" as part of the Food Product Design track in the SupplySide West Education Program. Her session will take place on Tuesday, Oct. 6, from 3 to 3:50 p.m. at Mandalay Bay in Las Vegas. Visit http://west.supplysideshow.com/edu-more.aspx for more information and to get registered.
References:
1. Morse N. “Lipid-lowering and anti-inflammatory effects of palmitoleic acid: Evidence from preclinical and epidemiological studies." Lipid Tech. 2015;27:107-111.
2. Maguire LS et al. “Fatty acid profile, tocopherol, squalene and phytosterol content of walnuts, almonds, peanuts, hazelnuts and the macadamia nut." Int J Food Sci Nutr. 2004;3:171-178.
3. Teleszko M et al. “Analysis of Lipophilic and Hydrophilic Bioactive Compounds Content in Sea Buckthorn (Hippophaë rhamnoides L.) Berries." J. Agric Food Chem. 2015;63:4120-9.
4. Hodson L, Karpe F. “Is there something special about palmitoleate?" Curr Opin Clin Nutr Metab Care. 2013;16:225-231.
5. Gong J et al. “Adipose tissue palmitoleic acid and obesity in humans: does it behave as a lipokine?" Am J Clin Nutr. 2011;93:186-91.
6. Bernstein A M et al. “Purified palmitoleic acid for the reduction of high-sensitivity C-reactive protein and serum lipids: a double-blinded, randomized, placebo controlled study." J Clin Lipidol. 2014;8:612-617.
7. Duckett S K et al. “Palmitoleic acid reduces intramuscular lipid and restores insulin sensitivity in obese sheep." Diabetes Metab Syndr Obes. 2014; 7:553-563.
8. Garg ML, Blake RJ, Wills RB. “Macadamia nut consumption lowers plasma total and LDL cholesterol levels in hypercholesterolemic men." J Nutr. 2003;133:1060-3.
9. Garg ML et al. “Macadamia nut consumption modulates favourably risk factors for coronary artery disease in hypercholesterolemic subjects." Lipids. 2007;42:583-7.
10. Curb J D et al. “Serum lipid effects of a high-monounsaturated fat diet based on macadamia nuts." Arch Intern Med. 2000;160:1154-1158.
11. Bolsoni-Lopes A et al. “Palmitoleic acid (n-7) increases white adipocyte lipolysis and lipase content in a PPARα-dependent manner." Am J Endocrinol Metab. 2013;305:E1093-1102.
12. Maedler K et al. “Distinct effects of saturated and monounsaturated fatty acids on beta-cell turnover and function." Diabetes. 2001;50:69-76.
13. Yang, Z et al. “Chronic administration of palmitoleic acid reduces insulin resistance and hepatic lipid accumulation in KK-Ay Mice with genetic type 2 diabetes." Lipids Health Dis. 2011;10:120. doi: 10.1186/1476-511X-10-120.
14. Sauma L et al. “PPAR-gamma response element activity in intact primary human adipocytes: effects of fatty acids." Nutrition. 2006;1:60-8.
15. Yang Z et al. “Oral administration of omega-7 palmitoleic acid induces satiety and the release of appetite-related hormones in male rats." Appetite. 2013;65:1-7.
16. Volk B M et al. “Effects of Step-Wise Increases in Dietary Carbohydrate on Circulating Saturated Fatty Acids and Palmitoleic Acid in Adults with Metabolic Syndrome." PLoS One. 2014; 9(11): e113605. doi:10.1371/journal.pone.0113605.
17. Lehtonen H M et al. “Different berries and berry fractions have various but slightly positive effects on the associated variables of metabolic diseases on overweight and obese women." Eur J Clin Nutr. 2001;65:394-401.
18. Larmo P S et al. “Effects of sea buckthorn and bilberry on serum metabolites differ according to baseline metabolic profiles in overweight women: a randomized crossover trial." Am J Clin Nutr. 2013;98:941-951.
19. Rodhe Y et al. “The effect of sea buckthorn supplement on oral health, inflammation, and DNA damage in hemodialysis patients: a double-blinded, randomized crossover study." J Ren Nutr. 2013;23:172-179.
20. Yang B. et al. “Effects of dietary supplementation with sea buckthorn (Hippophaë rhamnoides) seed and pulp oils on atopic dermatitis." J Nutr Biochem. 1999;10:622-630.
21. Johansson A K et al. “Sea buckthorn berry oil inhibits platelet aggregation." J Nutr Biochem. 2000;11:491-495.
About the Author
You May Also Like